Why Semaglutide Is Changing the Cardiovascular Conversation
GLP-1 medications like Semaglutide are often described as “weight-loss drugs.” That description isn’t wrong, but it’s incomplete. What’s becoming increasingly clear is that these therapies influence cardiovascular health in ways that go beyond the number on the scale. This distinction matters: weight is visible, cardiovascular risk is not.
And some of the most meaningful benefits of GLP-1 therapy may be happening beneath the surface, inside the arteries, the heart, and the metabolic systems that quietly shape our long-term cardiovascular outcomes.

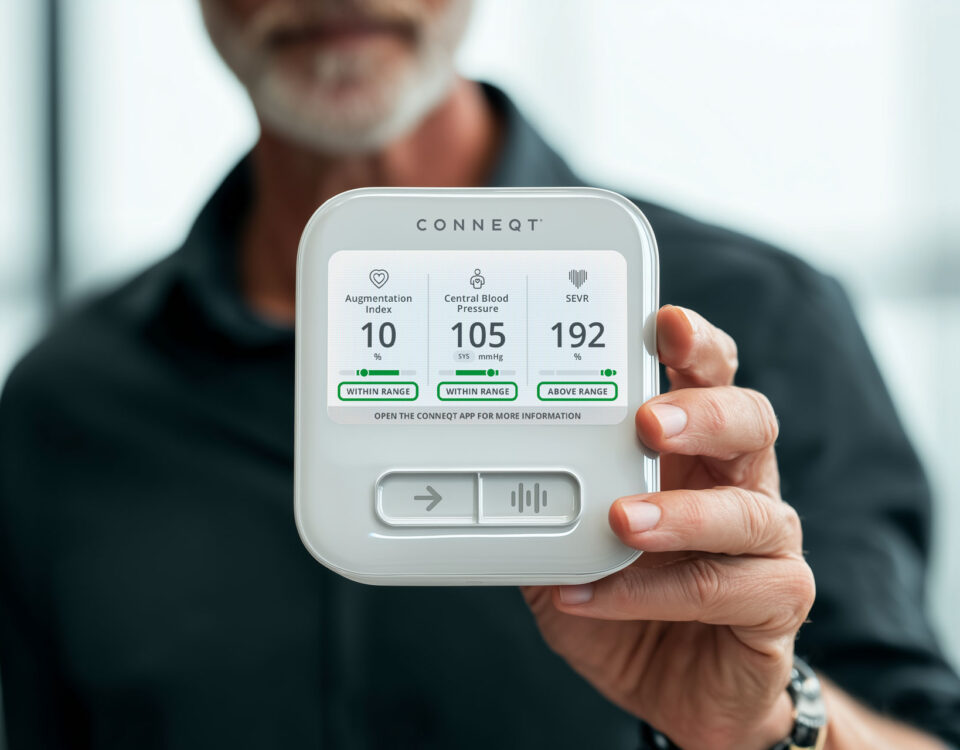
Medical Grade, Accurate, FDA-Cleared Heart Insights.
Save 20% on checkout with code VITALITY
More Than Appetite Control
Let’s start with a quick recap.
GLP-1 is a hormone your body naturally releases after eating. It helps regulate hunger, digestion, and blood sugar. GLP-1 medications are longer-acting versions of this signal, which is why they reduce appetite and support sustained weight loss.
But GLP-1 receptors aren’t limited to the gut or pancreas where we might intuitively expect them to be. They’re also found in blood vessels, the heart, and the kidneys. This broad distribution helps explain why people taking Semaglutide often experience improvements in blood pressure, metabolic health, and cardiovascular risk markers, not just reduced calorie intake.
This is the first key shift in perspective: GLP-1 medications are system-level metabolic therapies, not simply appetite suppressants.
Why Fat Loss From GLP-1 Medications Help the Heart
Clinical trials consistently show that Semaglutide leads to 10-15% total body weight loss in many individuals, even without diabetes.
But cardiovascular health depends less on how much weight you lose and more on what kind of weight you lose.
Visceral fat, the fat stored deep in the abdomen around vital organs, plays a major role in:
- Chronic inflammation
- Insulin resistance
- Elevated blood pressure
- And arterial stiffening
Reducing visceral fat improves how blood vessels function and lowers strain on the heart. When GLP-1 therapy is combined with lifestyle changes improvements in cholesterol, blood pressure, and other cardiometabolic markers become even more pronounced and may help explain why cardiovascular benefits observed during therapy often appear larger than what weight loss alone would predict.
Cardiovascular Protection That Goes Beyond Weight Loss
The strongest evidence for this comes from the SELECT trial, which studied patients with preexisting cardiovascular disease and overweight or obesity, but without diabetes. Participants taking Semaglutide experienced fewer heart attacks, strokes, and cardiovascular deaths compared with placebo.
What stood out was that these benefits:
- Appeared across a wide range of body sizes
- Were only partly explained by weight loss
- And persisted even when changes in body fat were modest
Follow-up analyses confirmed that improvements in cardiovascular outcomes could not be fully attributed to changes in body weight or waist circumference alone.
This suggests Semaglutide may directly improve vascular function, inflammation, and cardiac workload, all key drivers of long-term heart disease.
The Arterial Health Connection
Most people are familiar with blood pressure readings taken at the arm. But the pressure that the heart experiences, known as central blood pressure, along with the stiffness of the arteries, is more closely linked to heart damage and future cardiovascular events than arm readings alone.
As arteries stiffen with age, inflammation, and metabolic stress, pressure waves created during each heartbeat bounce back toward the heart instead of being smoothly absorbed by the arterial system. This increases the workload on the heart with every beat and accelerates long-term cardiovascular wear and tear.
Emerging evidence suggests GLP-1 therapies like Semaglutide may positively influence this process. Studies indicate these medications may help arteries remain more flexible, reduce the intensity of pressure waves returning to the heart, and lower the overall stress placed on the heart during each cardiac cycle.
Taken together, these effects point to meaningful improvements in arterial health, a critical but often overlooked factor in cardiovascular risk. While changes in weight and cholesterol are easier to measure, healthier arteries may be one of the most important ways GLP-1 therapy supports long-term heart protection.
The Trade-Off: Weight Loss Without a Plan Can Cost Muscle
Although the cardiovascular benefits of GLP-1 therapy are well supported, weight loss achieved with these medications is not composed exclusively of fat mass. Evidence indicates that a meaningful proportion of weight reduction (~25-40%) may involve lean tissue, including skeletal muscle, particularly in the absence of adequate nutritional intake or strength training.
Because skeletal muscle plays a central role in glucose regulation, metabolic resilience, physical function, and healthy aging, unintended losses may have implications beyond changes on the scale.
This does not diminish the therapeutic value of GLP-1 medications but instead underscores the importance of viewing weight loss through a broader physiological lens that accounts for body composition and long-term cardiometabolic health.
Other Important Considerations When Using GLP-1 Therapy
By design, GLP-1 medications alter appetite regulation, gastric emptying, and satiety signaling. In some individuals, particularly early in treatment, these physiological effects may be accompanied by gastrointestinal symptoms such as nausea or early fullness. The intensity and duration of these effects vary widely between individuals and can influence both tolerance and adherence over time.
Beyond tolerability, sustained appetite suppression introduces an additional consideration: reduced energy intake may inadvertently compromise nutritional adequacy if not carefully monitored. From a cardiometabolic perspective, preservation of lean mass and metabolic function remains important during weight loss, particularly when reductions occur rapidly or over extended periods.
For these reasons, GLP-1 therapy is best viewed as one component of a broader, supervised health strategy, one that considers nutrition, physical activity, body composition, and long-term cardiovascular risk together, rather than focusing on body weight alone.
A Cardiovascular Lens on GLP-1 Therapy
Semaglutide and other GLP-1 medications represent a meaningful shift in how we approach cardiometabolic risk. They don’t just help people lose weight; they help address upstream drivers of cardiovascular disease, including visceral fat, vascular dysfunction, and metabolic stress.
But the real opportunity lies in how these tools are used.
When combined with strength, nutrition, and long-term lifestyle changes, GLP-1 therapy can support healthier arteries, a more resilient heart, and lower cardiovascular risk over time. When used in isolation, it risks trading short-term weight loss for long-term muscle and metabolic health.
Editorial note
This article reflects the independent clinical perspective and interpretation of current research by the author. It is provided for educational purposes and is not intended to replace individualized medical advice or clinical decision-making.